Staphylococcus epidermidis | Microbiology Unknown Paper
Call Us Now
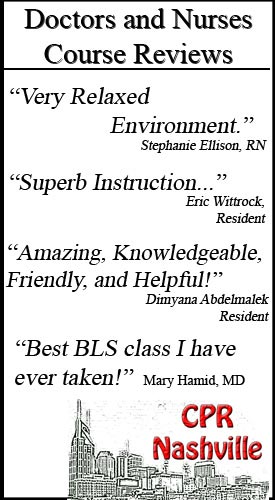
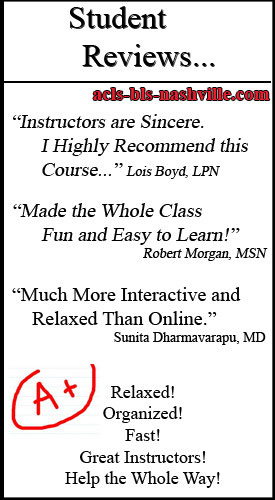
Get the Best CPR Class in Nashville Today!
MICROBIOLOGY UNKNOWN LAB REPORT
Kayla Cook
April 30, 2013
General Microbiology
INTRODUCTION
Understanding and distinguishing microorganisms from one another is a necessary step when trying to recognize how they play a part in not only humans but in the world. By identifying a microorganism, a patient can be diagnosed and treated, an organism can be studied, and antibiotics can be created. This unknown identification of bacterium was done in order to enforce and reiterate the process of using different methods used throughout the semester, in order to identify two different microorganisms.
MATERIALS AND METHODS:
The lab instructor passed out a tube of bacterium, known as an unknown, labeled number 120. The methods that have been learned and practiced throughout the entire semester were used in order to identify this particular unknown. The procedures that were followed throughout this identification can be found in the laboratory manual by McDonald Et.al (1), unless noted within this lab report.
Call Us Now
Get the Best CPR Class in Nashville Today!
The first step that was done was taking a Trypticase Soy Agar (TSA) plate, and using the quadrant streak method as described in the lab manual, the unknown was streaked onto the plate. This process was done in order to attempt to separate the two different bacteria contained in the unknown test tube. After two days, the plates had been incubated and grown in attempt to produce isolated colonies. Unfortunately, only one bacterium had been isolated, while the other did not grow on the Trypticase Soy Agar plate. The first individual colony that was isolated was separated onto a new TSA plate and streaked using the quadrant streak method to grow a pure culture. In order to separate the second bacterium from the original unknown broth tube, the first step was repeated. This step took the original test tube that contained the unknown and used the quadrant streak method to streak the unknown onto the plate. Once each Trypticase Soy Agar plate was incubate for two more days, the first agar plate now contained a pure culture and the second plate had isolated both bacteria. The second bacterium was then streaked on a Trypticase Soy Agar plate in order to grow a pure culture after two days of incubation. The pure culture of the first bacterium was placed in the refrigerator to prevent overgrowth. After two more days, the second bacterium had been separated and was now a pure culture.
Once each bacterium had successfully grown a pure culture on a Trypticase Soy Agar plate, a Gram stain was performed on each to determine the reaction. This process was completed twice in order to observe accurate results when Gram staining each bacterium. After the Gram stain had been completed, specific biochemical tests were performed on each bacterium in order to correctly identify each one. The biochemical tests were chosen based on the unknown identification tables that were handed out by the instructor. Given that unknown #120 contains two different bacteria, this was the time when separate steps were taken for each bacterium.
Unknown #120 “A” was determined to be a Gram-negative rod, the bacterium was streaked onto a MacConkey agar plate for a Lactose test to be performed. Not all of these tests were performed by the methods listed in the lab manual by McDonald et al. (1).
Table 1 lists the test, purpose, reagents, observations, and results.
All of the following tests were performed on this unknown:
- Lactose Test
- Urea Test
- Simmon’s Citrate Test
- Methyl Red Test
- Voges-Proskauer Test
Unknown #120 “B” was determined to be Gram-positive cocci, the bacterium was then inoculated into a Nitrate test tube for a Nitrate test to be performed. Note all of these tests were performed by the methods listed in the lab manual by McDonald et al. (1).
Table 2 lists the test, purpose, reagents, observations, and results.
- Nitrate Test
- Urea Test
- Catalase Test
- Methyl Red Test
- Mannitol Test
RESULTS:
Unknown #120 “A” contained a medium, cloudy cream-colored colony on a Trypticase Soy Agar plate. After verifying that the bacterium was a Gram-negative rod, the bacterium was streaked onto a MacConkey agar plate for a Lactose test to be performed. Table 1 lists all of the biochemical tests, purposes, reagents, observations, and results. The results are also shown in flow chart form.
Table 1: Test Information and Results of Unknown #120: “A”
|
TEST |
PURPOSE |
REAGENTS |
OBSERVATIONS |
RESULTS |
|
Gram Stain
|
To determine the Gram reaction of bacterium | Crystal violet, Iodine, Alcohol, Safranin | Pink rods |
Gram Negative rods |
|
Lactose Test
|
To determine if the bacterium can ferment lactose | None | Colonies appear to be a pink/red color | Positive Lactose Test |
|
Urea Test
|
To determine if the bacterium has the ability to hydrolyze urea using the enzyme urease | None |
No color change, Yellow color broth |
Negative Urea Test |
|
Simmon’s Citrate Test
|
To determine if the bacterium can use citrate as its sole carbon source | None |
No color change, Media stayed green |
Negative Simmons Citrate Test |
|
Methyl Red Test
|
To determine if the bacterium produces acids in glucose fermentation | Methyl Red | Color change from a light yellow to a cherry red. | Positive Methyl Red Test |
| Voges-Proskauer Test | To determine if the bacterium produce acetyl methyl carbinol | Barritt’s A & B |
Color did not change, yellow broth |
Negative Voges-Proskauer Test |
FLOWCHART (Removed Due to Formatting Issues with Blog)
UNKNOWN #120 “A”
Unknown #120 “A” – Escherichia coli
Unknown #120 “B” contained a small, clear-colored colony on a Trypticase Soy Agar plate. After verifying that the bacterium was Gram-positive cocci, the bacterium was inoculated into a Nitrate test tube for a Nitrate test to be performed. Table 1 lists all of the biochemical tests, purposes, reagents, observations, and results. The results are also shown in a flow chart form.
Table 2: Test Information and Results of Unknown #120: “B”
|
TEST |
PURPOSE |
REAGENTS |
OBSERVATIONS |
RESULTS |
|
Gram Stain
|
To determine the Gram reaction of bacterium | Crystal violet, Iodine, Alcohol, Safranin | Purple cocci |
Gram Positive cocci |
|
Nitrate Test
|
To determine if the bacterium is capable of reducing nitrate to nitrate or other nitrogenous compounds | Nitrate I & II, Zinc | Broth turned red after adding Nitrate I & II | Positive Nitrate Test |
|
Urea Test
|
To determine if the bacterium has the ability to hydrolyze urea using the enzyme urease | None | Color change, from yellow to pink | Positive Urea Test |
| Catalase Test | To determine if the bacterium can tolerate oxygen and produce catalase | Hydrogen Peroxide | Bubbling | Positive Catalase Test |
|
Methyl Red Test
|
To determine if the bacterium produces acids in glucose fermentation | Methyl Red | Color change from a light yellow to a cherry red. | Positive Methyl Red Test |
| Mannitol Test | To determine if the bacterium can ferment mannitol | None | No color change, mannitol nonfermenter | Negative Mannitol Test |
FLOWCHART (Removed Due to Formatting Issues with Blog)
UNKNOWN #120 “B”
DISCUSSION/CONCLUSION:
Unknown #120 “A”- Escherichia coli
- The test results of the biochemical tests help to determine the final identification for the bacterium, Escherichia coli. After performing a Gram stain that determined the bacterium was a Gram negative rod, the unknown identification table was utilized. There were five options of Gram negative rods that the bacterium could be. These options included Escherichia coli, Klebsiella pneumoniae, Enterobacter aerogenes, Proteus vulgaris, and Pseudomonas aeruginosa. By using the identification table, it helped to eliminate various organisms that did not fit the test results. For example, the Lactose test was determined to be positive, which then narrowed down the options to only three different organisms. This is why the identification was made after a Gram stain and five biochemical tests were done.
- Yes, the correct identification of the organism, Escherichia coli, was made after all the test results were observed.
- The only issues that came up during the identification of Escherichia coli was during the Gram stain process. The first time the Gram stain was performed, the Gram-negative rods did not show up clearly after the Safranin was added in the last step of the Gram stain method. This could have been because the Safranin did not stay on the slide for the correct amount of time. To fix this problem, another Gram stain was done which verified that this organism was Gram-negative rods. Repeating specific tests, it helps accurately determine that the results of each test were precise.
- Background Information on Escherichia coli:
As the Bergey’s Manual states, Professor Theodor Escherich was the first person to isolate and characterize Escherichia in 1885 (2). In 1935, the first outbreak of diarrhea among infants occurred from a strain of Escherichia coli (6). The Foundations of Microbiology textbook states, “Probably the most widely studied bacteriophages are those of the intestinal bacterium Escherichia coli” (3). This bacterium inhabits the intestinal tract of humans and many warm-blooded mammals (5). The Centers for Disease Control and Prevention state that most Escherichia coli is harmless and is many times an important part of a healthy intestinal tract of a human being (4). Kenneth Todar, PhD informs readers that this bacterium is the head of the bacterial family, Enterobacteriaceae. These enteric bacteria are facultative anaerobic Gram-negative rods, which live intestinal tracts of animals (6). This bacterium is part of a human’s normal flora in the intestinal tract. E.coli has been said to be, “crucial in the digestion of food, and is our principal source of vitamin K and B-complex vitamins” (5). However, some Escherichia coli can make humans sick. At times, E. coli can cause diarrhea, urinary tract infections, respiratory illness, pneumonia, and many other illnesses (4). Worldwide a strain of E. coli called O157:H7 is one of the most harmful (6). It was said to arose when Escherichia coli was infected with a virus carrying genes coding for the toxin Shigalike. (5). “This toxin can destroy cells in the intestinal tract and, if they enter the bloodstream, can impair or destroy the kidneys and the liver” (5). Of course, this disease caused by Escherichia coli can be avoided when using proper techniques including hand washing, washing raw foods, thorough cooking of meat, and avoiding unpasteurized milk (5).
Unknown #120 “B”- Staphylococcus epidermidis
- The test results of the biochemical tests helped to determine the final identification of the bacterium, Staphylococcus epidermidis. After performing a Gram stain that determined the bacterium was Gram positive cocci, the unknown identification table was utilized. Based on the table, there were only three different organisms that unknown “B” could be. These three options were Staphylococcus aureus, Staphylococcus epidermidis, and Enterococcus faecalis. One test that narrowed down the options was the results of the Urea test. The Urea test result was positive showing that the bacterium was capable of hydrolyzing urea using urease. This determined that most likely the bacterium was Staphylococcus epidermidis. However, in order to make sure these were accurate results, other tests were performed. Each of these tests that were executed after the Gram stain, helped to identify the second organism.
- No, the identification of the organism was incorrect the first time. This was because the Mannitol test was performed two times during lab testing. The first time the Mannitol test was performed, it turned out to be a negative result. However, the test was repeated towards the end of identification and the results were different. The second time, the results showed a positive result for mannitol metabolism. It is possible that this could be because the pure culture or the Mannitol Salt Agar (MSA) was contaminated. After understanding that the second test result was incorrect for mannitol, the correct identification of the organism was determined.
- With the Gram positive organism, Staphylococcus epidermidis, a few problems occurred during the identification process. The first problem began when trying to separate the unknowns in order to get individual colonies. After two days of incubation, the Trypticase Soy Agar plate only grew the Gram negative bacteria. To fix this problem, another quadrant streak was done on a TSA plate using the original unknown test tube. This time, after a two day period of incubation, the Gram positive and Gram negative bacteria were present. It was visible to the eye that there were two different species of bacteria present on the agar plate. The only other problem that was encountered was inaccurate test results of the Mannitol test the second time. However, this could be from a possible contamination when streaking the bacteria on the plate. Or it could be from contamination of the pure culture. Fortunately, these problems were handled and in the end both organisms were identified from the original unknown broth tube #120.
REFERENCES:
- Lab Manual for General Microbiology. Revised Ed. St. Louis: St. Louis Community College, 2011. Print.
- Breed, Robert S., E. G. D. Murray, Nathan R. Smith, et al. Berge’ys Manual of Determinative Bacteriology. Baltimore: 1957. Web. 18 Apr. 2013.
- Talaro, Kathleen P., and Barry Chess. Foundations of Microbiology. 8th ed. Boston: McGraw Hill Companies, 2012. Print.
- “E. Coli (Escherichia Coli).” Centers for Disease Control and Prevention. Centers for Disease Control and Prevention, 03 Aug. 2012. Web. 17 Apr. 2013.
- “Escherichia coli.” World of Microbiology and Immunology. Ed. K. Lee Lerner and Brenda Wilmoth Lerner. Vol. 1. Gale Cengage, 2003. eNotes.com. 17 Apr, 2013
http://www.enotes.com/escherichia-coli-reference/
- Todar, Kenneth. “Pathogenic E. Coli.” Pathogenic E. Coli. N.p., 2008. Web. 17 Apr. 2013.
These papers are written by future healthcare providers, such as nursing students. All healthcare providers are required to have CPR classes to become AHA certified. If you need an American Heart Association CPR class visit BLS, ACLS, PALS classes, Nashville