Overview of Pediatric Cardiac Emergencies
When a child experiences a cardiac emergency outside of a hospital setting, the swiftness and effectiveness of the response can mean the difference between life and death. Pediatric cardiac arrest is a devastating event, and unlike adults, where heart problems are often the cause, children typically suffer cardiac arrest due to respiratory issues or shock. This critical difference highlights the importance of a specialized approach to their care.
Importance Pediatric Chain of Survival
Understanding the pediatric out-of-hospital chain of survival is not just helpful; it is absolutely vital for parents, caregivers, educators, and anyone who might find themselves in a position to help a child in distress. The steps within this chain are interconnected and interdependent, each playing a crucial role in improving outcomes for young patients. Statistics on pediatric cardiac arrest outcomes underscore this urgency, revealing that prompt, correct intervention significantly boosts survival rates and reduces the likelihood of long-term neurological impairment.
Understanding the Pediatric Chain of Survival Concept
The concept of the chain of survival provides a clear, sequential framework for emergency response, and its origins lie in the recognition that a series of coordinated actions can dramatically improve survival from cardiac arrest. For pediatric cases, this chain is specifically adapted to address the unique physiological and developmental characteristics of children
Pediatric Chain of Survival Concept
Each “link” in this chain represents a critical step that must be executed effectively and without delay. If even one link is weak or broken, the entire chain is compromised, lessening the chances of a positive outcome. The interconnectedness of these steps means that early, decisive action in one stage directly impacts the success of subsequent stages. It is a testament to the idea that emergency response is a team effort, beginning with the bystander and continuing through the most advanced medical care.
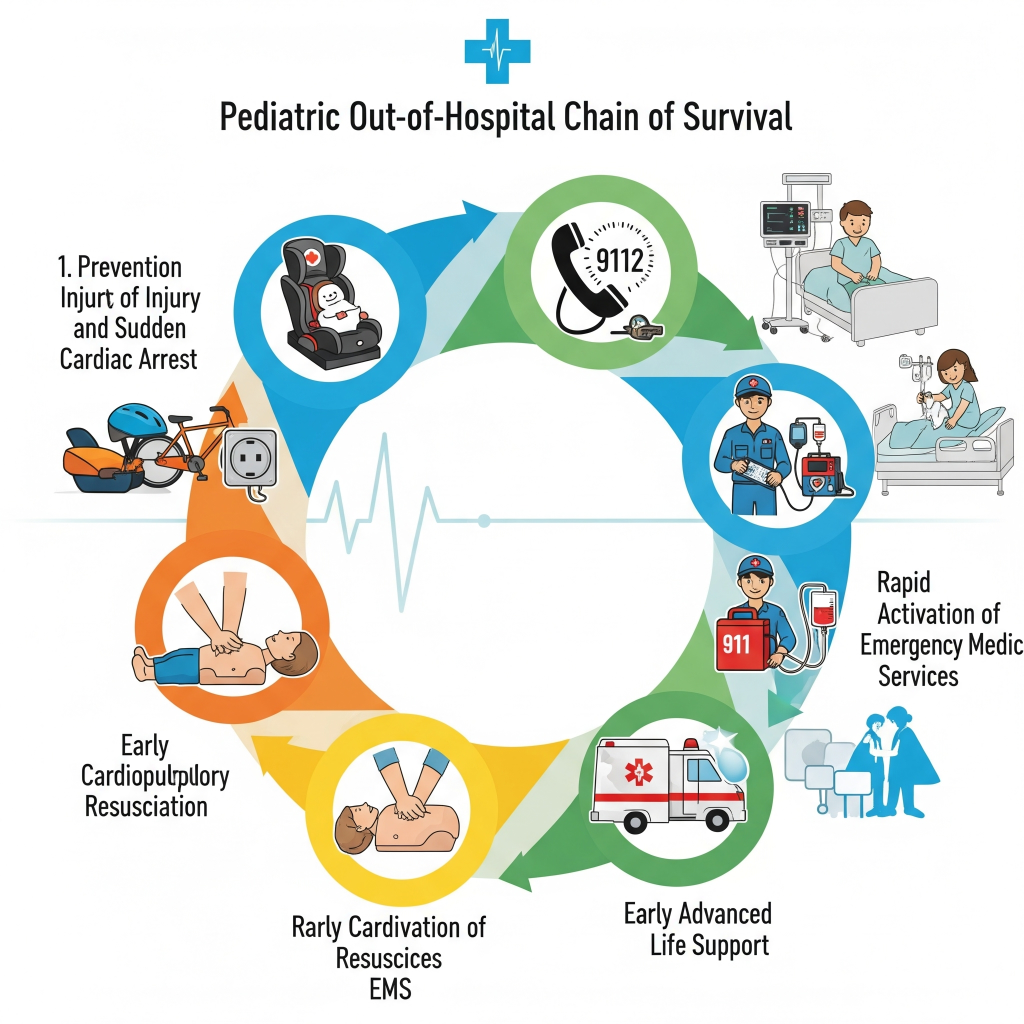
The Five Steps of the Pediatric Out-of-Hospital Chain
The pediatric out-of-hospital chain of survival consists of five essential steps, each building upon the last to create a continuous and effective response.
Prevention
The very first link in this life-saving sequence is prevention. This step is arguably the most crucial because it aims to avert cardiac emergencies before they even occur. Prevention in pediatrics often involves addressing the common causes of cardiac arrest in children, such as accidental injuries, suffocation, drowning, and severe respiratory illnesses.
Educating parents and caregivers on child safety, proper supervision, and recognizing early signs of distress can significantly reduce the incidence of these tragic events. For instance, promoting safe sleep practices for infants, securing homes to prevent accidents, and advocating for swimming lessons can all contribute to a preventative approach.
Early Recognition and Activation of Emergency Response
Following prevention, the second step is early recognition and activation of emergency response. Once a child shows signs of a cardiac emergency, time becomes a critical factor. Recognizing the symptoms of respiratory distress, unresponsiveness, or an absent pulse quickly allows for immediate action.
Upon recognition, activating the emergency medical services, typically by calling 911 or the local emergency number, is paramount. Providing clear and concise information to the dispatcher, including the child’s age, condition, and location, ensures that help arrives as swiftly as possible. This step emphasizes the importance of basic first aid knowledge and the confidence to act decisively in a crisis.
High-Quality CPR with Emphasis on Chest Compressions
The third vital link in the chain is high-quality cardiopulmonary resuscitation, or CPR, with a strong emphasis on chest compressions. Once emergency services have been activated, immediate bystander CPR can bridge the critical time gap until professional help arrives. High-quality CPR for children involves specific techniques tailored to their smaller bodies and developing physiology.
This includes correct hand placement, appropriate compression depth and rate, and allowing for full chest recoil between compressions. The focus on chest compressions is because they are crucial for maintaining blood flow to the brain and other vital organs, even in the absence of effective breathing. Even if a bystander is unsure about rescue breaths, effective chest compressions alone can significantly improve survival rates.
Advanced Life Support by Emergency Medical Services
The fourth step involves advanced life support provided by emergency medical services. Once paramedics or other trained medical professionals arrive on the scene, they bring a higher level of medical intervention. This advanced life support includes the administration of medications, advanced airway management, and the use of defibrillation if appropriate.
These interventions are designed to stabilize the child’s condition, address the underlying cause of the cardiac arrest, and prepare them for transport to a medical facility. The seamless transition from bystander care to professional medical care is essential for maintaining the momentum of the rescue effort.
Integrated Post-Cardiac Arrest Care
Finally, the fifth and often overlooked step is integrated post-cardiac arrest care. Survival from cardiac arrest is not merely about restarting the heart; it also involves ensuring the best possible neurological outcomes and overall recovery. This stage begins as soon as the child’s heart rhythm is restored and continues through their hospitalization and rehabilitation.
Integrated post-cardiac arrest care involves a multidisciplinary approach, including therapeutic hypothermia, careful management of oxygenation and ventilation, and addressing any underlying medical conditions that contributed to the arrest. The goal is to minimize secondary brain injury and support a full recovery, allowing the child to return to their normal life with minimal long-term effects.
Why Each Step Matters: The Science Behind the Chain
The science behind the chain of survival powerfully illustrates why each step truly matters. Survival statistics for pediatric cardiac arrest dramatically increase with each successful link in the chain. Conversely, delays in any single step can have devastating consequences. For instance, a delay in initiating CPR can lead to irreversible brain damage within minutes due to a lack of oxygen. Similarly, waiting too long to activate emergency services can delay the arrival of advanced medical care, reducing the window of opportunity for effective intervention. This highlights the time-sensitive nature of pediatric cardiac emergencies and the critical role of immediate and coordinated action. Each second counts, and every completed step contributes significantly to a positive outcome.
Special Considerations for Pediatric Cases
Special considerations are often necessary for pediatric cases due to the distinct differences between children and adults. Age-specific techniques are crucial for administering CPR and other life-saving measures effectively. For example, the depth and force of chest compressions vary significantly between infants, young children, and adolescents. Moreover, the common causes of cardiac arrest in children differ from those in adults, with respiratory failure and shock being more prevalent than primary cardiac events. Understanding these nuances allows responders to tailor their approach and provide the most appropriate care for the child’s specific situation. Recognizing the subtle signs of distress in children, which may differ from adults, is also a vital skill for caregivers.
Training and Preparedness
Training and preparedness form the backbone of a successful pediatric emergency response. The importance of CPR certification for caregivers, including parents, teachers, and childcare providers, cannot be overstated. These certifications provide individuals with the essential skills and confidence to act quickly and effectively in an emergency. Community education programs also play a significant role in spreading awareness and empowering more people with life-saving knowledge. Furthermore, schools and childcare facilities have a responsibility to be prepared for such emergencies, implementing clear protocols and ensuring staff are adequately trained.
CPR Nashville: Your Partner in Pediatric Emergency Preparedness
Organizations like CPR Nashville offer vital resources, including initial certifications and renewals in BLS for Healthcare Providers, ACLS, PALS, and CPR and First Aid courses. Their emphasis on stress-free and hands-on training ensures that participants gain practical skills and retain information effectively. PALS (Pediatric Advanced Life Support) certification is particularly important for healthcare providers who frequently care for children, while family CPR and First Aid courses empower parents and guardians.
FAQs
1. What is the pediatric out-of-hospital chain of survival?
The pediatric out-of-hospital chain of survival is a series of critical actions designed to improve survival rates for children experiencing cardiac emergencies outside of medical facilities. It includes prevention, early recognition, and activation of emergency response, high-quality CPR, rapid defibrillation when appropriate, effective advanced life support, and integrated post-cardiac arrest care.
2. How does the pediatric chain of survival differ from adult protocols?
Pediatric protocols emphasize prevention as the first link since cardiac arrest in children is often caused by respiratory issues rather than primary cardiac problems. Children require different compression-to-ventilation ratios, appropriately sized equipment, and specialized medication dosing. The approach focuses more on airway management and breathing support compared to adult protocols.
3. What training do I need to effectively implement the pediatric chain of survival?
Healthcare providers should obtain certification in Pediatric Advanced Life Support (PALS), Basic Life Support (BLS), and CPR. These certifications teach proper pediatric assessment, age-appropriate resuscitation techniques, medication administration, and post-resuscitation care. Regular recertification ensures skills remain current with the latest guidelines.
4. Can parents and non-healthcare providers learn pediatric emergency response skills?
Yes, parents, teachers, and community members can learn pediatric CPR and first aid through certified training programs. While they may not perform advanced interventions, they can provide crucial early recognition, call for help, and perform basic life support until professional help arrives. This early intervention is vital in the chain of survival.
Call to Action
Ready to save a child’s life? Master the pediatric chain of survival with expert training at CPR Nashville.
Get certified in PALS, BLS, and pediatric CPR through our American Heart Association-approved courses. Our stress-free, hands-on training ensures you’re confident and prepared for pediatric emergencies.
Enroll today and become the crucial first link in a child’s survival.
📞 Contact CPR Nashville – Nashville’s premier AHA training site
✅ Initial certifications and renewals available
✅ Small class sizes for personalized attention
✅ Experienced instructors with real-world expertise