When someone’s heart stops beating, every second counts. Understanding CPR and rescue breathing techniques can mean the difference between life and death. Immediate CPR can double or triple survival chances after cardiac arrest, making it one of the most critical skills you can learn. This guide will help you master the essential techniques of rescue breaths and CPR.

Understanding the Difference Between CPR and Rescue Breathing
Many people use these terms interchangeably, but CPR and rescue breathing serve different purposes in emergency response.
Cardiopulmonary resuscitation is a life-saving technique used during cardiac arrest to maintain blood flow and oxygenation to vital organs. CPR combines two essential actions: chest compressions and rescue breaths. The compressions manually pump blood through the body, while rescue breaths deliver oxygen to the lungs.
Rescue breathing, also called mouth-to-mouth resuscitation, focuses solely on providing ventilation to someone who has stopped breathing but still has a pulse. In respiratory arrest situations where the patient has a pulse but is not breathing, rescue breathing should be provided until spontaneous respiration resumes.
The key distinction lies in the heart’s activity. If the heart has stopped (cardiac arrest), you perform full CPR with both compressions and breaths. If the heart is still beating but breathing has ceased (respiratory arrest), rescue breathing alone may suffice.
What is the Rescue Breathing Rate for CPR?
Proper ventilation rates are critical for effective resuscitation. According to recent American Heart Association guidelines, the rescue breathing rate varies depending on the situation and the victim’s age.
For Adults with a Pulse but Not Breathing
For adult patients who are not breathing normally but have a pulse, rescuers should provide 1 breath every 6 seconds, which equals 10 breaths per minute. Each breath should last about one second and produce visible chest rise.
During Active CPR
When performing CPR, the compression-to-ventilation ratio is 30:2 for adults. Healthcare providers and trained rescuers should use chest compressions and mouth-to-mouth breathing at a ratio of 30 compressions to 2 breaths. This pattern continues until emergency medical services arrive or the person shows signs of life.
For Children and Infants
The ventilation rates differ for younger patients. Children require approximately 12-20 rescue breaths per minute (one breath every 3-5 seconds), while infants need 20-30 breaths per minute (one breath every 2-3 seconds). These faster rates account for children’s higher metabolic needs and smaller lung capacities.
With an Advanced Airway
Once healthcare providers place an advanced airway such as an endotracheal tube, the approach changes. Rescuers deliver continuous chest compressions without pausing, while providing ventilations at a rate of one breath every six seconds (10 breaths per minute).
How to Perform Rescue Breathing in CPR
Mastering the technique of rescue breathing ensures you deliver effective ventilations during an emergency. Here’s the proper step-by-step approach:
Step 1: Ensure Scene Safety and Check Responsiveness
Before approaching the victim, verify the area is safe. Tap the person’s shoulder and shout loudly to check for responsiveness. If there’s no response, immediately call 911 or have someone else call while you begin care.
Step 2: Position the Victim and Open the Airway
Lay the person flat on their back on a firm surface. Use the head-tilt, chin-lift maneuver to open the airway. Place one hand on the forehead and gently tilt the head back while lifting the chin with two fingers of your other hand. If you suspect a neck or spine injury, use the jaw-thrust technique instead.
Step 3: Check for Breathing
Look for chest rise, listen for breath sounds, and feel for air movement. Take no more than 10 seconds for this assessment. Gasping or irregular breathing does not count as normal breathing.
Step 4: Deliver Rescue Breaths
If the person is not breathing normally, begin rescue breaths:
- Seal the airway: Pinch the person’s nose shut while maintaining the head tilt
- Create a seal: Place your mouth completely over the victim’s mouth
- Give the breath: Blow steadily for about one second
- Watch for chest rise: The chest should visibly rise with each breath
- Allow exhalation: Remove your mouth and let the chest fall completely before giving the next breath
Step 5: Continue with Proper Ratio
If performing CPR, give 30 chest compressions at a rate of 100-120 per minute, followed by 2 rescue breaths. Compress the chest at least 2 inches deep for adults. Continue this cycle until help arrives or the person responds.
Using Barrier Devices
While mouth-to-mouth works in emergencies, barrier devices like pocket masks or bag-valve masks are preferred when available. These devices reduce disease transmission concerns and often provide more effective ventilation.
Understanding the 5 Rescue Breaths in CPR
The concept of “5 rescue breaths” appears in specific emergency scenarios, particularly those involving children and drowning victims. Understanding when and why to use this approach can improve outcomes in these critical situations.
Initial Rescue Breaths for Drowning Victims
The 2024 American Heart Association guidelines for drowning victims recommend that trained rescuers should initiate CPR by giving two rescue breaths followed by 30 chest compressions. This modified sequence recognizes that drowning causes cardiac arrest through oxygen deprivation rather than a primary heart problem.
The “Phone Fast” Approach for Children
For unresponsive children, trained rescuers should provide approximately 5 cycles of CPR (about 2 minutes) before leaving to activate emergency services if alone. This approach differs from the “phone first” protocol for adults because most pediatric cardiac arrests result from respiratory problems rather than sudden cardiac events.
Why the Difference Matters
Cardiac arrest following drowning is most often due to a hypoxic mechanism, making rescue breathing important to increase the likelihood of return of spontaneous circulation. When the body lacks oxygen, quickly restoring breathing takes priority over immediate chest compressions.
Research shows that victims of non-cardiac arrest (such as drowning, drug overdose, or respiratory failure) benefit significantly from early rescue breaths. The blood in their bodies may still contain oxygen, but it cannot circulate without chest compressions, and new oxygen cannot enter without ventilation.
The Science Behind Rescue Breaths and CPR
Recent studies continue to refine our understanding of optimal resuscitation techniques. The American Heart Association updates its guidelines every five years based on the latest research from the International Liaison Committee on Resuscitation.
2024 Guidelines Updates
The most recent updates, published in November 2024, emphasize several key points:
Compression quality matters: Adequate depth (at least 2 inches for adults), appropriate rate (100-120 per minute), complete chest recoil between compressions, and minimal interruptions all contribute to better outcomes.
Ventilation effectiveness: Each rescue breath should take about one second and produce a visible chest rise. Excessive ventilation can harm the victim by increasing pressure in the chest and reducing blood return to the heart.
Early defibrillation: The AED can be used if available, but CPR should be started before using an AED in drowning cases.
Gender Disparities in CPR
According to a Resuscitation Science Symposium study, men are 1.23 times more likely to receive bystander CPR in public locations, and their survival chance is 23 percent higher compared to women. This disparity likely stems from bystander hesitation about performing chest compressions on women. Understanding this bias can help rescuers overcome it and provide equal care to all victims.
Common Mistakes to Avoid
Even trained rescuers can make errors that reduce CPR effectiveness. Watch out for these common pitfalls:
Ventilating too fast or too forcefully: Excessive ventilation can cause gastric inflation, increase the risk of vomiting, and reduce the effectiveness of chest compressions. Each breath should be delivered over one second with just enough volume to make the chest rise.
Inadequate chest compressions: Compressions that are too shallow, too slow, or interrupted too frequently will not maintain adequate blood flow. Push hard and push fast, allowing complete chest recoil between compressions.
Delaying CPR: The longer cardiac arrest continues without CPR, the lower the survival chances become. Don’t waste time checking multiple times for breathing or pulse—if you’re unsure, start compressions immediately.
Poor hand placement: For adults, place the heel of your hand on the center of the chest between the nipples. For children, use one or two hands depending on their size. For infants, use two fingers placed just below the nipple line.
Take Action: Get Certified Today
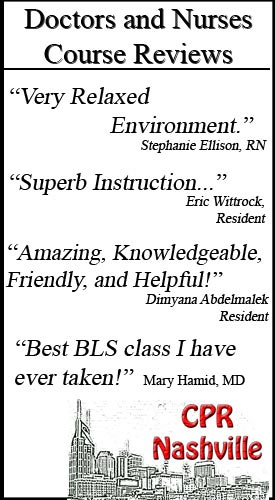
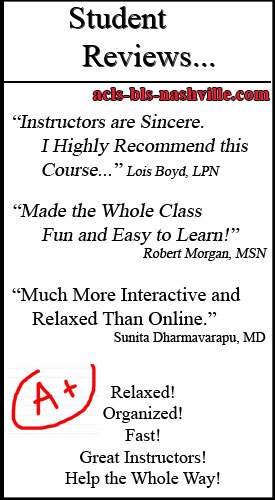
Reading about CPR provides valuable knowledge, but hands-on training with expert instructors makes the real difference in emergency situations. Proper training helps you develop muscle memory, gain confidence, and learn to respond effectively under pressure.
CPR Nashville offers comprehensive training that meets American Heart Association standards. As an official AHA training site, we provide initial certifications and renewals in BLS for Healthcare Providers, ACLS, PALS, and CPR and First Aid courses. All our classes are stress-free and hands-on, ensuring you gain practical skills you can use confidently.
Whether you need CPR certification in Nashville for your job or want to be prepared for family emergencies, our experienced instructors guide you through every technique. Healthcare professionals can maintain their credentials with BLS certification in Nashville through our convenient renewal courses.
Don’t wait for an emergency to wish you had these skills. Enroll in a certification course today and gain the confidence to save a life tomorrow. Visit CPR Nashville or call to schedule your training session. Your decision to get certified could make you someone’s hero when they need it most.