When it comes to pediatric emergencies, specialized training is essential to provide the best possible care for young patients in critical situations. Pediatric Advanced Life Support (PALS) training equips healthcare providers with the skills necessary to recognize and respond effectively to a wide range of emergencies in infants and children. This type of training, offered by AHA-certified centers like CPR Nashville, focuses on the unique challenges of treating pediatric patients and ensures that medical professionals are prepared for any scenario that may arise. In this guide, we’ll delve into the common pediatric emergencies covered in PALS training, illustrating the importance of specific protocols and advanced knowledge when treating children.
Respiratory Emergencies
Respiratory issues are among the most common emergencies that children face, and PALS training dedicates considerable time to addressing these situations. Children’s smaller airways make them more susceptible to breathing problems, and prompt, accurate responses are crucial to prevent deterioration.
Upper Airway Obstruction
Upper airway obstruction is a frequent concern, often resulting from conditions like croup, foreign body aspiration, or anaphylaxis. Croup, a viral infection causing inflammation around the vocal cords, leads to the characteristic barking cough and difficulty breathing. Another common cause, foreign body aspiration, happens when an object blocks the airway, often requiring immediate intervention. Anaphylaxis, a severe allergic reaction, can cause swelling that obstructs the airway, demanding quick administration of epinephrine and other supportive measures.
Lower Airway Obstruction
Lower airway emergencies, such as asthma, bronchiolitis, and pneumonia, also require rapid recognition and response. Asthma attacks, which involve the constriction of airways, are often managed with bronchodilators and steroids, while bronchiolitis, typically caused by RSV, requires careful monitoring and oxygen therapy. Pneumonia, an infection in the lungs, may require antibiotics and supportive care based on the severity.
Recognition and Assessment
Recognizing signs of respiratory distress, such as increased work of breathing, abnormal breath sounds, and altered respiratory rates, is a critical part of PALS training. Identifying these signs early can significantly impact the outcome, as respiratory issues are a leading cause of cardiac arrest in children.
Cardiac Emergencies
Cardiac emergencies in pediatric patients are less common but require precision and advanced skills when they do occur. Pediatric cardiac arrest demands high-quality CPR, with proper techniques specific to the child’s age and size. PALS emphasizes the importance of age-appropriate compression depths and effective compression-to-ventilation ratios to ensure adequate blood flow and oxygenation during resuscitation efforts.
Arrhythmias
Arrhythmias, or abnormal heart rhythms, also pose serious threats. Bradycardia, or a slow heart rate, and tachycardia, or a fast heart rate, can both be signs of underlying issues that require immediate intervention. PALS covers a range of arrhythmias, including supraventricular and ventricular tachycardia, as well as pulseless electrical activity (PEA), which can be life-threatening if not treated promptly.
Shock States
PALS training also addresses different types of shock states, which are critical conditions that compromise blood flow and oxygenation. Hypovolemic shock, resulting from fluid loss, septic shock from infection, and cardiogenic shock from heart dysfunction all require tailored interventions to restore adequate circulation.
Neurological Emergencies
Seizures
Neurological issues such as seizures and altered mental status are also focal points of PALS training. Seizures, particularly febrile seizures in young children, are common but can be alarming and sometimes lead to more serious conditions like status epilepticus, where the seizure lasts too long and requires immediate intervention.
Altered Mental Status
Altered mental status in children can stem from various causes, including hypoglycemia, poisoning or toxicity, and head trauma. Recognizing the signs of these issues, such as confusion, lethargy, and irritability, helps responders address the root cause quickly. Hypoglycemia, or low blood sugar, is particularly dangerous as it can quickly escalate if not treated. PALS training covers how to assess and manage these neurological emergencies efficiently.
Critical Care Interventions
Airway Management
PALS provides healthcare professionals with training in crucial interventions necessary to stabilize pediatric patients. Effective airway management techniques are a primary component, as maintaining an open airway is vital in respiratory and cardiac emergencies. Techniques such as bag-mask ventilation, advanced airway placements, and appropriate oxygen therapy are essential skills covered in the program.
Vascular Access
Vascular access is another critical intervention, as administering medications or fluids often requires an IV or intraosseous access. PALS training offers guidance on placing IVs in children, as well as using intraosseous access when veins are difficult to locate.
Medication Administration
Administering emergency medications accurately is a must in pediatric care, as dosages vary based on a child’s weight and age. PALS teaches dosing calculations and safe administration routes to ensure medication effectiveness and patient safety.
Team Dynamics and Communication
Role Assignment
Effective teamwork is essential during pediatric emergencies, and PALS training emphasizes role assignment and communication skills.
The team leader is responsible for coordinating actions and making critical decisions, while each team member has specific roles that contribute to the overall success of the intervention.
Effective Communication
Closed-loop communication, where orders are clearly stated and confirmed, helps avoid misunderstandings and ensures that everyone is on the same page.
Family-Centered Care
Family-centered care is another important aspect covered in PALS, as parents or guardians may be present during resuscitation efforts. Maintaining open communication with the family, explaining the situation and treatment plan, and offering emotional support are all vital elements that enhance the care experience for both the patient and their loved ones.
Post-Resuscitation Care
Stabilization
The role of healthcare providers does not end after resuscitation, as stabilizing the patient and preparing for transport is crucial for a positive outcome. Monitoring vital signs and conducting ongoing assessments allow the medical team to detect any changes in the patient’s condition and respond accordingly.
Transport Considerations
Transport considerations, such as when to transfer the patient to a specialized facility, and the necessary preparations for transport, are also important elements in post-resuscitation care. PALS training provides guidelines on ensuring that patients receive consistent, high-quality care from the initial response through transport to advanced care facilities.
Conclusion
Pediatric emergencies require specialized knowledge and quick, effective responses, and PALS training ensures healthcare providers are well-prepared to handle these critical situations. Through training on respiratory, cardiac, and neurological emergencies, and vital interventions, PALS helps build a solid foundation of skills that save young lives.
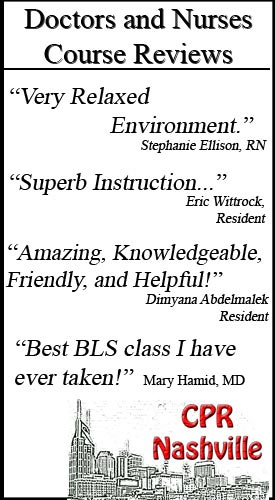
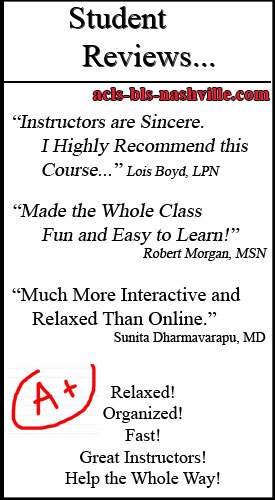
CPR Nashville is dedicated to offering high-quality, American Heart Association-certified PALS courses that prepare participants to confidently face pediatric emergencies with expertise and compassion.
For those looking to enhance their pediatric emergency skills, consider enrolling in a PALS course at CPR Nashville. Certification and renewal options are available to ensure that healthcare providers stay current with the latest techniques and protocols.
Visit CPR Nashville’s website or contact us directly for course scheduling, registration information, and additional details on our comprehensive training options. Join us to make a difference in the lives of children and families through expert care and life-saving interventions