Understanding Synchronized Cardioversion in Emergency Cardiac
The heart’s electrical system is a finely tuned marvel, but when it misfires, the results can be catastrophic. Every year, countless individuals experience life-threatening cardiac arrhythmias—irregular heartbeats that disrupt the normal flow of blood and threaten immediate collapse. For healthcare providers working in emergency settings, rapidly assessing and treating these rhythms is not just a medical procedure; it is a life-saving imperative.
This is where the skill of performing synchronized cardioversion becomes indispensable, serving as a rapid, definitive intervention to restore a stable, functional rhythm. Understanding this procedure is fundamental for anyone certified in Advanced Cardiac Life Support, offering a critical tool to stabilize patients who are rapidly deteriorating due to organized, yet dangerously fast, heart rhythms.

What is Synchronized Cardioversion?
Synchronized cardioversion is defined as a therapeutic dose of electrical current delivered to the heart to convert an abnormal, symptomatic rhythm into a normal sinus rhythm. Unlike other electrical interventions, the core concept hinges on delivering the electrical energy in precise synchronization with the patient’s R-wave, which is the peak of the QRS complex on an electrocardiogram.
This meticulous timing is essential because delivering a shock during the vulnerable repolarization period, known as the T-wave, could inadvertently trigger ventricular fibrillation, a fatal rhythm.
When Synchronized Cardioversion is Performed
The goal of synchronized cardioversion is purely conversion, aiming to reset the heart’s intrinsic pacemaker and allow it to take over at a safer rate. The procedure is indicated for a range of persistent, unstable tachyarrhythmias where the patient still has a pulse, including atrial fibrillation with a rapid ventricular response, atrial flutter, supraventricular tachycardia, and ventricular tachycardia with a pulse. These interventions can be performed either in an emergency setting, where a patient is showing signs of instability like hypotension or altered mental status, or as an elective, scheduled procedure when the rhythm is known but is not immediately life-threatening. The decision to proceed is always driven by patient stability and follows strict protocols outlined in the latest ACLS guidelines.
The Two Methods of Cardioversion
When a patient requires a rapid rhythm conversion, there are two primary methods available to the clinician: electrical and pharmacological cardioversion. The most immediate and often most effective method in an emergency is electrical cardioversion, which utilizes an external defibrillator or cardioverter device to deliver a direct current shock.
Method 1: Electrical Cardioversion (Synchronized DC Cardioversion)
Electrode pad placement is crucial for maximizing current flow across the heart, typically using an anterior-posterior or anterior-lateral configuration, and specific energy levels are selected based on the type of arrhythmia being treated. For instance, less energy, often between 50-100 Joules, may be used for rhythms like atrial flutter or SVT, while higher doses, such as 120-200 Joules for biphasic devices, are reserved for refractory atrial fibrillation. The step-by-step process requires careful calibration and is often taught through hands-on practice.
Method 2: Pharmacological Cardioversion
In contrast, pharmacological cardioversion involves administering antiarrhythmic medications to achieve chemical conversion. Common drugs utilized in this method include Amiodarone, which works by affecting multiple ion channels, or Flecainide and Propafenone, often used in patients with structurally normal hearts. Chemical cardioversion is generally preferred when the patient is clinically stable and not severely symptomatic, or when the rhythm is of recent onset. While this method avoids the need for sedation and electrical shock, its success rate can be lower, and the conversion process takes much longer to complete compared to the immediate effect of electrical therapy.
Comparison of Methods
Ultimately, the choice between electrical cardioversion and drug therapy is a critical clinical decision, factoring in the patient’s immediate condition, the specific arrhythmia, and the clinical setting, all of which are thoroughly covered in comprehensive ACLS training programs.
The Cardioversion Procedure: Step-by-Step Guide
Before delivering a synchronized cardioversion shock, thorough pre-procedure preparation is mandatory to ensure both patient safety and procedural success.
Pre-Procedure Preparation
This process begins with a comprehensive patient assessment, securing informed consent whenever the patient is conscious and able to provide it. Because the procedure is painful, conscious sedation is almost always necessary, meaning medications must be prepared and administered by a qualified professional before the shock is delivered. Safety protocols are paramount and include checking all equipment, ensuring proper gel-pad adherence, and removing any sources of oxygen from the immediate area to prevent fire hazards. Team communication must be crystal clear throughout the preparation phase.
Procedure Steps
The procedure itself follows a standardized sequence. Once the patient is positioned and the electrodes are placed, the crucial step of device synchronization is performed by pressing the ‘sync’ button on the cardioverter, which allows the machine to detect the R-wave. The provider then selects the appropriate energy level based on the current rhythm. Before pressing the charge button, a firm, clear verbal warning, the “Clear” protocol, is announced to ensure all personnel are safely away from the patient and the bed. The shock is then delivered, and the provider must maintain the button press until the synchronized discharge occurs. Immediately following the shock, a rapid post-shock assessment of the patient’s rhythm and vital signs is performed to confirm successful conversion or determine the need for subsequent attempts.
Post-Procedure Care
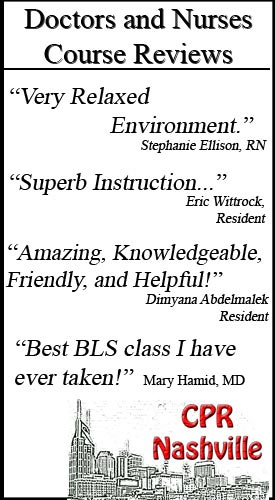
Post-procedure care involves continuous cardiac monitoring to detect recurrence of the arrhythmia, careful documentation, and management of potential complications, which is a key focus of the training received at a certified site like CPR Nashville.
Cardioversion vs. Defibrillation: Critical Differences
It is impossible to master emergency cardiac care without clearly understanding the difference between synchronized cardioversion and defibrillation. While both use electrical energy, their indications and delivery methods are fundamentally distinct, a difference that can mean the difference between life and death.
Here are the key distinctions:
- Synchronization timing: Cardioversion is synchronized to the R-wave peak to avoid the vulnerable T-wave, whereas defibrillation is immediate, unsynchronized energy delivery.
- Target rhythm: Cardioversion is indicated for organized rhythms where a pulse is present, such as Atrial Fibrillation or Ventricular Tachycardia with a pulse; defibrillation is reserved for disorganized, pulseless rhythms like Ventricular Fibrillation and pulseless Ventricular Tachycardia.
- Energy level: Cardioversion typically uses lower initial energy settings, while defibrillation requires the highest available energy setting (often 200 Joules biphasic) from the start.
- Patient status: Cardioversion is often performed on conscious or sedated patients with a pulse; defibrillation is performed on unconscious, pulseless patients.
Clinical Decision Making
Clinical decision making begins with rapid and accurate rhythm recognition and, most importantly, a thorough pulse assessment.
Common Mistakes and Prevention
A common and dangerous mistake is misidentifying a rhythm or failing to properly activate the synchronization feature on the device, which converts the procedure into a potentially harmful defibrillation. Through rigorous training in both BLS Certification and ACLS protocols, providers learn to recognize these critical differences and prevent common errors.
Tips for Rhythm Identification
Essential Rhythm Recognition Skills
A reliable intervention begins with a reliable interpretation. Essential rhythm recognition skills are not just theoretical; they require a practiced ability to interpret the 12-lead ECG, focusing on key features like the rate, the regularity, the morphology of the P-waves and QRS complexes, and the QRS width.
Identifying a narrow complex tachycardia that requires synchronized cardioversion, such as SVT, versus a wide complex rhythm like VT with a pulse, is the bedrock of proper management.
While modern cardiac monitors offer valuable technology assistance and computer interpretation, no machine can replace the clinical correlation and judgment of a trained provider who can assess the patient’s presentation against the tracing. ACLS courses place a strong emphasis on hands-on rhythm practice to build these vital skills under stress-free conditions.
FAQs About Synchronized Cardioversion
What is the difference between synchronized cardioversion and defibrillation?
Synchronized cardioversion delivers a controlled electrical shock timed to the heart’s QRS complex to avoid the vulnerable refractory period, making it safer for patients with a pulse and organized cardiac rhythms, such as atrial fibrillation or SVT. Defibrillation, on the other hand, delivers an unsynchronized shock and is used for life-threatening arrhythmias like ventricular fibrillation or pulseless ventricular tachycardia when there is no organized rhythm to synchronize with.
When should synchronized cardioversion be performed?
Synchronized cardioversion is indicated for patients with unstable tachycardia who have symptoms such as hypotension, altered mental status, chest pain, or acute heart failure. It’s commonly used to treat atrial fibrillation, atrial flutter, supraventricular tachycardia (SVT), and stable ventricular tachycardia with a pulse. The procedure can be performed electively for stable patients or emergently when the patient becomes hemodynamically unstable.
What are the risks and complications of synchronized cardioversion?
While generally safe when performed correctly, synchronized cardioversion carries some risks, including skin burns at paddle sites, embolic events (particularly stroke if clots dislodge from the heart), arrhythmias following the procedure, and, in rare cases, deterioration to ventricular fibrillation if the shock is delivered at the wrong time. Proper sedation can also carry risks of respiratory depression. These risks are why the procedure should only be performed by trained healthcare providers with appropriate monitoring equipment available.
Do I need special training to perform synchronized cardioversion?
Yes, synchronized cardioversion should only be performed by healthcare providers who have received proper training in advanced cardiac life support. ACLS certification provides comprehensive training on recognizing unstable rhythms, operating the cardioversion equipment, selecting appropriate energy levels, and managing potential complications. Healthcare providers should maintain current certifications and regularly practice these lifesaving skills to ensure competency in emergencies.
Call to Action
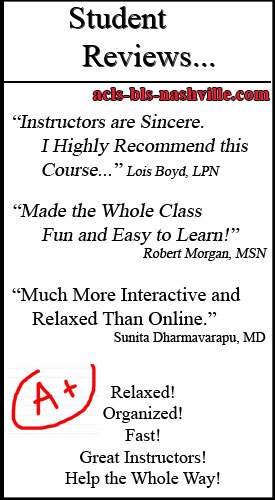
Master lifesaving cardiac interventions, such as synchronized cardioversion! Enroll in ACLS classes in Nashville at CPR Nashville, an American Heart Association training site. Whether you need CPR certification in Nashville or want to advance your skills with ACLS, PALS, or BLS for Healthcare Providers, our stress-free, hands-on courses prepare you for real-world emergencies. Get certified with the Best CPR in Nashville today!