What are BLS Algorithms?
In life-threatening emergencies, knowing exactly what to do—without hesitation—can be the deciding factor between life and death. Basic Life Support (BLS) algorithms serve as structured, step-by-step guides for healthcare providers and trained responders, ensuring swift and systematic action during cardiac or respiratory arrest. These algorithms are more than checklists—they’re evidence-based tools that save lives.

Why BLS Algorithms Matter
BLS refers to the immediate care provided to someone experiencing cardiac arrest, respiratory arrest, or airway obstruction. It includes chest compressions, rescue breathing, and defibrillation when necessary. The use of BLS algorithms ensures a consistent approach, allowing providers to respond quickly, accurately, and confidently, even under intense pressure. Whether you’re the only responder or part of a team, these protocols guide you in delivering high-quality care that improves outcomes and increases survival rates.
The BLS Primary Survey Algorithm
The reason BLS algorithms matter so much lies in their ability to reduce variability in care. Emergencies are stressful and fast-moving. Algorithms remove uncertainty, helping responders take action rooted in best practices. By following a standardized process, healthcare providers can deliver life-saving interventions with greater precision, improving patient outcomes across various healthcare settings.
The CAB Approach
The foundation of BLS is the CAB sequence: Compressions, Airway, Breathing. This order reflects a critical shift in recent years, placing the highest priority on high-quality chest compressions. When cardiac arrest is suspected, start by checking for responsiveness and normal breathing. If the patient is unresponsive and not breathing normally, immediately begin chest compressions. After 30 compressions, provide 2 rescue breaths while ensuring the airway is open. This cycle—30 compressions to 2 breaths—continues until advanced help arrives or the patient recovers.
Step-by-Step Implementation
Before initiating the CAB steps, ensure the scene is safe. Then, assess the patient for responsiveness and breathing. Activate emergency medical services and, if an AED is available, retrieve it immediately. Begin compressions without delay. This sequence is simple but powerful, designed to maximize the chances of restoring circulation and oxygenation in the early minutes of cardiac arrest.
Adult BLS Algorithm
The Adult BLS Algorithm begins with recognizing cardiac arrest, marked by unresponsiveness, absence of breathing, and no detectable pulse within 10 seconds.
CPR Sequence
Start chest compressions at a rate of 100 to 120 per minute and a depth of at least 2 inches. Allow complete chest recoil after each compression. Maintain a compression-to-ventilation ratio of 30:2. Limit interruptions to compressions as much as possible.
AED Integration
As soon as an AED is available, apply it and follow its prompts. If a shockable rhythm is detected, deliver the shock and immediately resume CPR. If no shock is advised, continue compressions. Regular rhythm checks are performed every two minutes, following AED or manual defibrillator prompts. Always resume CPR immediately after a shock or rhythm analysis.
Pediatric BLS Algorithm
Pediatric BLS algorithms adapt the CAB approach to the unique needs of infants (under 1 year) and children (1 year to puberty). Cardiac arrest in children is often due to respiratory failure, making effective ventilation a top priority. Compression depth and rate are adjusted: at least 1.5 inches for infants and 2 inches for children, still at 100 to 120 compressions per minute. If two rescuers are present, the compression-to-breath ratio changes to 15:2 for children and infants.
In infants, use the two-thumb encircling technique for compressions if two rescuers are available. For solo rescuers, two fingers on the sternum are used. Proper airway positioning is essential to ensure effective ventilation. Pediatric airway anatomy requires gentler head tilt and chin lift maneuvers to avoid airway obstruction.
Modified CPR Techniques
Special scenarios in pediatrics, such as choking, require age-specific interventions. For infants, use back slaps and chest thrusts. For children over one year, abdominal thrusts are the preferred method. Rescuers must be alert to the emotional dynamics when parents are present and balance medical care with compassionate communication.
Team-Based BLS Algorithms
Team-based BLS is most effective when roles are clearly defined. One person should assume leadership, directing compressions, airway management, and AED use. Rotate compressors every two minutes to prevent fatigue and ensure consistent compression quality. Effective teams practice closed-loop communication—giving clear instructions and confirming they’ve been carried out.
Roles and Responsibilities
After an event, a structured debrief helps teams reflect, identify areas for improvement, and reinforce successful practices. Debriefs are key to continuous quality improvement and maintaining high standards in emergency care.
Algorithm Decision Points and Modifications
Knowing when to start and stop BLS is also part of the algorithm. Start BLS when a patient is unresponsive, not breathing normally, and pulseless. However, do not begin resuscitation if the patient has valid Do Not Resuscitate (DNR) orders or clear signs of irreversible death, such as rigor mortis. Stop BLS if return of spontaneous circulation (ROSC) occurs, advanced care takes over, or the rescuer is physically unable to continue safely.
Special Circumstances
There are also special situations that require algorithm modifications. Hypothermia may require prolonged CPR efforts, and defibrillation attempts may be delayed until the patient is warmed. In cases of drug overdose, airway protection and ventilation are particularly critical. For trauma-related cardiac arrest, addressing hemorrhage and tension pneumothorax may take priority.
Quality Metrics and Monitoring
To ensure high-quality CPR, BLS providers must focus on specific quality metrics. Compressions must be at the correct rate and depth, with full chest recoil. Interruptions should be minimized—ideally, the chest compression fraction (time spent doing compressions) should be over 80%.
Ventilation Quality
For ventilation, avoid excessive breaths or large volumes. Deliver just enough air to make the chest rise. Using a bag-valve mask requires a proper seal, correct rate (1 breath every 6 seconds in adults), and appropriate oxygen flow.
Technology Integration
Technology integration is increasingly important. Real-time feedback devices help rescuers adjust in the moment, measuring depth, rate, and hand placement. Post-event analysis tools allow teams to review performance and identify opportunities for improvement. These tools elevate both individual and team performance.
Common Algorithm Pitfalls and Solutions
Despite training, common pitfalls in BLS persist. These include shallow compressions, hyperventilation, over-long pulse checks, and lack of coordination. The best way to avoid these mistakes is through regular skills practice, simulation-based learning, and honest performance feedback. Even experienced providers benefit from refreshers to stay sharp and current with best practices.
Staying Current with BLS Guidelines
Staying up to date with BLS guidelines is essential. The American Heart Association (AHA) updates its guidelines every five years based on new research. Providers must renew certification typically every two years and are encouraged to participate in continuing education. For those who want to go further, advanced certifications like ACLS and PALS build on the foundational skills taught in BLS.
Conclusion
BLS algorithms offer a life-saving roadmap for responding to cardiac arrest and other emergencies. By following the CAB approach—Compressions, Airway, Breathing—rescuers can act quickly and confidently when seconds count. With a structured algorithm, effective teamwork, and high-quality skills, you can significantly improve a patient’s chance of survival.
Your role in the chain of survival is vital. From recognizing cardiac arrest to starting CPR and using an AED, your training makes a difference. Make sure you’re ready.
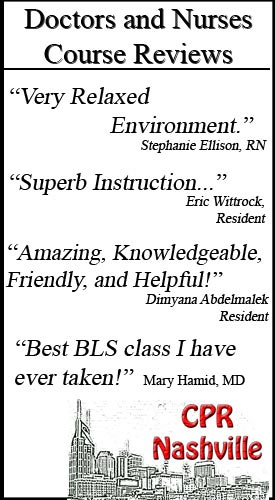
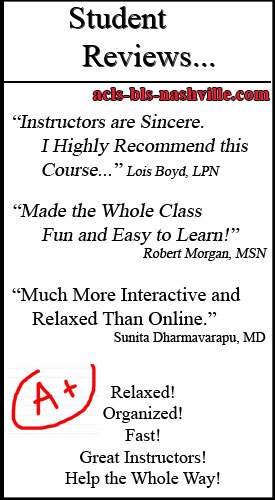
Transform your emergency response capabilities today. Contact CPR Nashville to enroll in our comprehensive BLS for Healthcare Providers course and join thousands of confident, capable healthcare professionals who trust our stress-free, hands-on training approach. Your patients’ lives may depend on the skills you learn with us.