UNKNOWN LAB REPORT
VERA KOZLOVA
MICROBIOLOGY
FALL 2012
Introduction
There are many purposes for identifying an unknown bacterium. One of the purposes for determination of the pathogenic microbes causing diseases is prescribing correct medication for treatment. Another purpose is to know if these pathogens are widespread in nature, inhabiting soil, water, and plants in order to find ways of how to prevent these infections. This experiment was done by applying methods for identification on unknown bacterium.
Materials and Methods
An unknown bacterium A with mixed culture containing 2 types of bacteria was handed out by the Lab instructor. The methods that have been learned were accomplished by separating and differentiating possible bacteria based on specific biochemical characteristics .The tests performed on unknown bacteria cultures were all used to determine the identity of the bacteria. Each of the tests provided some key information about the bacteria and how it functions. Not all the tests were done on every culture, however, as some of them were used only for gram -positive bacteria and some of them only for gram -negative bacteria. Tests were followed as stated in laboratory manual. The first step used to separate 2 types of bacteria for identification was making an isolation streak from the mixed culture on to Nutrient Agar plate, using the streak method described in Lab manual. It was made on purpose to obtain a pure culture containing one bacterium. After the plate was incubating for growing on the second day it was examined and the results were recorded. The Gram-stain was performed. It was hard to recognize whether it was Gram-positive or Gram-negative bacteria, because there was predominance of Gram-negative rod-shaped bacteria. The color of bacteria was pink, but there were a lot of purple spots. It was hard to see the exact shape and size of two different bacteria.
The identifying the unknown bacteria was started over again. The unknown tube A with mixed culture containing 2 types of bacteria was given out by the instructor again. The streak plate was made from original broth of mixed culture on the Nutrient Agar plate, using a method described in the lab manual. In order to be able to have a pure culture of unknown bacteria, this procedure was made. The plate was left in the incubator for 24 hours for growing. After observation of the plate, it was clear that there was a lot of growth. Some of that growth was taken for the making of another streak plate on Nutrient Agar, in order to isolate a pure colony. After the plate was taken from the incubator on the next day, the examination of growth was observed.
The next procedure was accomplished by the Gram stain. The color of bacteria was pink, but there were a lot of purple spots. It was hard to recognize exactly whether it was Gram-positive bacteria or Gram- negative bacteria.
The differential media, which allows to differrentiate bacteria base upon their metabolic activity and selective media. It allows the growth of certain kinds of bacteria and inhibits the growth of others .This media was used. For this test, the unknown A was taken and one streak on MSA agar plate and another streak on MacConkey agar plate was made. After the plates were incubated and grown, the morphology was observed. The agar plate MSA was completely clear with no appearance of growth. The result was negative. The MacConkey agar plate had a brick red color to it, which meant the lactose fermenter of the Gram – negative. This media inhibits Gram -positive. Some bacteria from the MacConkey agar plate was taken and a streak plate on Nutrient Agar was made. This required the use of the streak method described in the lab manual. The plate was incubated and grown. One more test was done to confirm that it was Gram-negative growing on the MacConkey agar plate. The Gram stain was completed and proved to be the red rods Gram-negative bacteria. Quality control bacteria were Gram stained along with the unknown to make sure that the Gram stain reaction was finished accurately. The elimination method was used and crossed out all the positive bacteria for the list on this test. Since unknown A was determined by Gram- negative rods the biochemical test was chosen from the unknown identification tables in the lab manual. All these tests were made by methods listed in the lab manual. The purpose ,reagents were listed by table1.
All of those tests were made on the Unknown A:
1. Urea test
2. Simmons Citrate
3. Methyl Red
4. Vogel- Proskauer
5. Glucose and lactose test.
6. Oxidase test
7. Casease test.
Urea test was accomplished. The unknown bacteria for production of enzyme urenease broke down the urea. The urea tubes contained pH indicator (phenol red), if positive, alkaline products changed color of broth from tan to pinkish-red. .If not,color stay the same and had negative results. After inoculation the tubes with the samples and incubation- the test of the media didn’t change the color of the broth. It was negative results on Urea test for Escherichhia coli, Enterobacter aerugenes and Pseudomomas aeruginosa.
For the Simmons Citrate test was used Simmons Citrate agar slant to test unknown A for citrate usage as the only carbon source. If positive for this test, bacteria produced the enzyme citrase, which broke down the citrate pH indicator bromthymol blue by turning media from green to blue on slant. After the incubation the slant turned to blue, which meant that had positive results on Klebsiella pneumoniae, Enterobacter aerogenes, and Pseudomonas aeruginosa.
For the next two tests,the same MR-VP medium was used, wich contained protein and glucose. These two tests were Methyl Red and Vogel-Proskauer. The Methyl Red detects acid as final end products of glucose fermentation. Production of acetoin from pyruvic acid. Acetoin gave a negative result with the Methyl Red test. The results for Unknown A were negative for Enterobacter aerogenes and Pseudomonas aeruginosa.
The Vogel-Proskauer test detects production of acetonin. Inoculated tubes with unknown A bacteria after the incubation gave a positive result for Enterobacter aerugenosa. .To test for oxidase the unknown A from Nutrient Agar was used. It didn’t have an appearance of purple a color,so the test for the Enterobacter aeruginosa was negative.
Next test was made on Glucose and lactose. For those tests the Kligler tubes were used wich contained a medium with a specific sugar “phenol red” a dye that changes color with pH. The broth changed color from red to yellow when bacteria fermented the sugar and produced acid. This test had positive result on Glucose because slant was red on top, which also showed a negative result on Lactose.
The tube with alternative unknown B bacteria was given out by the instructor. The first test that was needed to be completed was to streak the unknown B out on a Nutrient agar plate, using the streak method described in lab manual. After plate was incubated it had contaminated. Another streak plate from alternative solution B was made based on the of the use the streak method described in lab manual. Plate was placed in incubator.
One more test on Casein was done for Unknown A. The enzyme casease broke down the casein and absorbed the amino acids for use in metabolism. For positive result, this breakdown had been seen around bacterial growth, where white cloudiness appeared to be cleared. But there wasn’t any cleanse which meant the Enterobacter aerogenes were negative. The methods listed in the referenced lab manual were the bases upon which these tests were performed.
After the plate with bacteria B was incubated and grown the colony was appeared and Gram stain was made. The color of bacteria was purple rods of the Gram positive on the slide. After the Gram reactionwas figured out, biochemical tests were made. The biochemical tests were taken from the lab manual. The unknown B was recognized as Gram positive rod, a Methyl Red .The Methyl Red detects acid as final end products of glucose fermentation. When the pH indicator methyl red is added to these cultures, the tubes will turn bright red indicating the presence of acids. This gram positive rod had a positive result. The next oxidase test was made. To test for oxidase unknown B from Nutrient Agar was used. It didn’t have an appearance of purple color, so the test was negative on Bacillus Subtilis.
One more test was done on Casein for unknown B. The enzyme casease broke down the casein and absorbed the amino acids for use in metabolism. For positive result, this breakdown had been seen around bacterial growth where white cloudiness appeared to be cleared. The results for Casein were positive on Bacillus cereus. All those biochemical tests were on Gram- positive rod made from table listed in Lab- manual.
RESULTS – removed due to formatting issues with flowcharts
DISSCUSSION/CONCLUSION
After a few unlike tests it was decided that unknown B was Bacillus subtilis .After performing the Gram stain to figure out that the unknown was a Gram-positive rod. The bacteria grown on the Nutrient Agar plate were used for inoculating to all biochemical tests. Only the biochemical test on the casein test was wrong, but other tests were correct. The Casein test gave a false negative result .This was understandable because it didn’t match with the results of another test.
In conclusion the identification of unknown A was Enterobacter aerogenes .Based on the Gram stain the unknown A was a Gram-negative rod. The colony was separated from the MacConkey Agar plate to Nutrient agar plate. From agar plate the bacteria was taken for inoculation for all of the biochemical tests. The well-working results were given by the rest of the biochemical tests. It gave correct results from the beginning test with Urea to the end -with the Casein. It was narrowed down between two kind of negative bacteria. Results on glucose and lactose test especially determined that the Gram- negative was only for Enterobacter aerogenes. This is so, because Glucose was the only Gram- negative result for Enterobacter aerogenes.The well-working beochemical tests were confirmed by Oxidase and Casein. After all it was clear to see that the unknown A was Enterobacter aerogenes.
Enterobacter aerogenes is a bacterium that is nosocomial and pathogenic and causes opportunistic infections including most types of infections. It is a gram-negative rod shaped bacteria. E. aerogenes does not generally cause disease in healthy individuals and is generally found in the human gastrointestinal tract. It has been found to live in various wastes, hygienic chemicals, and soil.
The gram-negative bacteria inhabit a natural flora in the gastrointestinal tract of animals as well as humans and reside in soil, water, dairy products. Enterobacter species, particularly Enterobacter aerogenes, are important nosocomial pathogens responsible for various infections, including bacteremia; lower respiratory tract infections, infections in skin and soft-tissue, urinary tract infections (UTIs), endocarditis, intra-abdominal infections, CNS, and ophthalmic infections. Enterobacter species can also cause various community-accessed infections, including UTIs, skin and soft-tissue infections, and wound infections, among others.
Enterobacter species are well-known for their drug resistance, which is thought to have been amplified by the use of broad-spectrum cephalosporins in hospitals. E. aerogenes uses three mechanisms of resistance; inactivating enzymes, changes in drug targets, and the ability of drugs to enter and acquire in its cells.
Risk factors for nosocomial Enterobacter infections include hospitalization of greater than 2 weeks, invasive procedures in the past 72 hours, treatment with antibiotics in the past 30 days, and the presence of a central venous catheter. The crucial first step is the appropriate identification of the bacteria. Physicians treating patients with Enterobacter infections are advised to abstain certain antibiotics, particularly third-generation cephalosporins because resistant mutants can quickly come into sight.
Important practices such as hand hygiene and environmental decontamination are crucial to the prevention and control of E. aerogenes. Also, aseptic insertion of catheters and implanted devices will reduce transmission of the organism.
Works Cited
“Pathophysiology.” Enterobacter Infections. Bioquell, 30 2012. Web. 4 Dec 2012. <http://www.bioquell.com/technology/microbiology/enterobacter-aerogenes/>.
Enterobacter Infections. Medscape Reference, 30 2012. Web. 4 Dec 2012. <http://emedicine.medscape.com/article/216845-overview>.
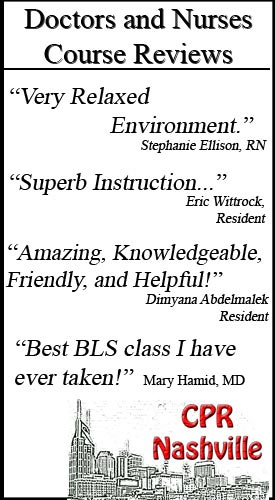
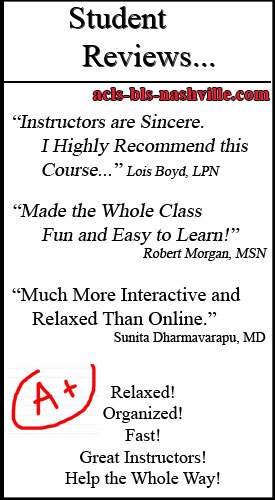
CPR classes in Nashville for nursing students, medical students, dental students, paramedics, etc